
OR
Black fungus’s surge in COVID-19 patients in India and lesson for Nepal
Published On: May 18, 2021 11:46 AM NPT By: Dr Rohit Saiju


Dr Rohit Saiju
The writer is a professor of Ophthalmology at NAMS and president of Nepal Ophthalmic Society.news@myrepublica.com
Black fungus affects individuals with low immunity like elderly people, cancer, diabetic and organ transplant patients. The incidence of black fungus is increasing in post COVID-19 patients because of the use of steroids, immunomodulatory drugs like Tocilizumab, and a prolonged use of humidified oxygen in hospitals.
It has developed as a trend and a challenge for the medical fraternity in these pandemic days. It is called black fungus or mucormycosis, the cases of which are on the rise in India. It is a rare and deadly fungal infection. It has been reported in several states in India, mostly in COVID-19 patients who survived the virus but now face a new battle. In the past decade, doctors have seen only a handful of cases in India. But in the past month, they reported hundreds of cases. The most common form of the infection seen among COVID-19 patients in India is rhinocerebralmucormycosis, an infection that starts in the sinuses and can spread to the brain.
This type of mucormycosis occurs more frequently among patients with diabetes, which is why health experts say cases are spiking in India where one in every six people has the chronic disease, according to the International Diabetes Federation Diabetes Atlas published in 2019. Diabetes is the number one risk factor for this as up to 75 percent of mucormycosis cases occur among COVID-19 patients with diabetes, with as many as 45 percent undiagnosed until they show up at the hospital. The Indian population has a high prevalence of uncontrolled diabetes due to the lack of routine screening and it is feared that the same scenario is prevalent in Nepal as well.
In pre-COVID times, this infection was quite rare in the world but since the pandemic, the cases have increased due to complications created by the virus. Last year only a few cases were reported from Gujarat and New Delhi but now the new virus mutants have triggered a surge in black fungus infection across the country. Cases have been reported from many states including our neighboring states like New Delhi, Uttar Pradesh, Bihar, Madhya Pradesh, Gujarat, Maharashtra, Telangana, Karnataka, Tamil Nadu, Rajasthan and other parts of India. Fungal infections are cropping up not only in India but in Europe, South America and the United States as well. However, instead of mucormycosis, which is less common outside of India, doctors are seeing cases of aspergillosis.The infection can cause blindness and even death if it reaches the brain.
Mucormycosis is caused by mucormycetes fungi which are present in our environment especially soil, decaying organic matter, damp and moist rooms, wet surfaces etc. Mucormycosis is an opportunistic fungal disease caused by molds belonging to the Rhizomucor species. They produce an encapsulated component of the fungus called spores which are protected from different unfavorable environmental conditions like heat and dryness. When we inhale the spores, it converts into an active vegetative cell and can grow and utilize our body tissue and feast on it. This fungus is rare but deadly if untreated or diagnosed late. On the basis of its location, it is classified into Rhino Orbito cerebral, pulmonary, Gastrointestinal, Cutaneous and disseminated forms.
Why it is common in COVID patients
Mucormycosis affects individuals with low immunity like elderly people, cancer, diabetic and organ transplant patients. The incidence of black fungus (mucormycosis) is increasing in post COVID-19 patients because of the use of steroids, immunomodulatory drugs like Tocilizumab, and a prolonged use of humidified oxygen in hospitals. Others who are at risk are those who have a prolonged stay in hospital ICUs and are yet to recover. The infection typically starts from the nose, paranasal sinuses, orbit (eye socket) and can travel to the brain in a short period. Once it reaches the brain, it is almost a death sentence as the mortality rate is as high as up to 96 percent.
If COVID-19 patients see any of the following symptoms, they must see a doctor at the earliest.
Pain in the eye or one side of the face, one side facial swelling with droopy eyelid, nasal or sinus congestion, black eschar around the nose, black lesion in nasal bridge, darkish nasal bleeding, severe headache and toothache, lack of eye movements and rapid deterioration in the vision. Chest pain and breathing difficulties occur if lungs are involved. Once it reaches the eye socket, usually blindness occurs due to the damage of one of the blood vessels supplying blood to the retina.

How do we protect ourselves from such infections
No use of steroid without the doctor’s prescription. Strict control of diabetes during or after COVID-19 period. Use clean, sterile water in oxygen humidifiers. Maintain personal hygiene including a thorough scrubbing and clean surroundings. Wear a mask all the time. Wear gloves and cover the body while outdoors.
Managing such cases is a big challenge. It involves the surgical removal of the entire infected and dead tissues by a team of ENT, Eye and neurosurgery and administering an antifungal drug called Amphotericin B daily for eight weeks. The cost of the drug and its scarcity make it another challenge for the treatment.
This COVID-19, steroid and diabetes triad converts the disease from virus to fungus problem and makes it more challenging for the doctors. We can understand that there is a big whistle blowing from our neighboring country and this problem will come to Nepal and we have to be prepared to deal with this. The suspected cases are requested to refer timely to tertiary hospitals or medical colleges where a team of Eye ,ENT Maxillofacial and neurosurgery can work together.
(The writer is a professor of Ophthalmology at NAMS and president Nepal Ophthalmic Society.)
You May Like This

Nepal’s COVID-19 test positivity rate, transmission rate almost double than that of India
KATHMANDU, May 9: Nepal’s COVID-19 test positivity rate and transmission rate are found almost double than that of India. ... Read More...
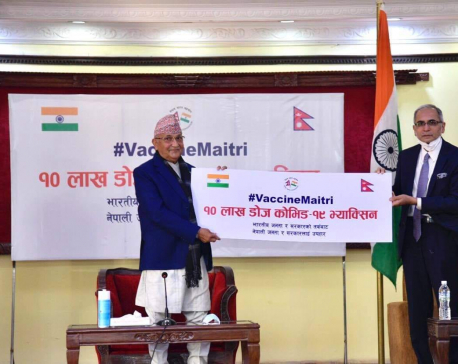
Half a million frontline workers to get two shots of ‘Covishield’ vaccine each in first phase
Health Ministry says vaccination drive against COVID-19 will start within a week ... Read More...

Govt prepares to inoculate health and sanitation workers in the first phase
India has decided to provide a limited amount of ‘Covishield’ for free within a week, according to Indian media outlets Read More...









Just In
- Forced Covid-19 cremations: is it too late for redemption?
- NRB to provide collateral-free loans to foreign employment seekers
- NEB to publish Grade 12 results next week
- Body handover begins; Relatives remain dissatisfied with insurance, compensation amount
- NC defers its plan to join Koshi govt
- NRB to review microfinance loan interest rate
- 134 dead in floods and landslides since onset of monsoon this year
- Mahakali Irrigation Project sees only 22 percent physical progress in 18 years









Leave A Comment