
OR
Superbugs will kill
Published On: May 27, 2018 01:30 AM NPT By: Samendra Prasad Sherchan & Binod Rayamajhee

Samendra Prasad Sherchan & Binod Rayamajhee
Sherchan is Assistant Professor at Department of Global Environmental Health Sciences, School of Public Health and Tropical Medicine, Tulane University, New Orleans. Rayamajhee is Research Faculty, Department of Infectious Diseases, Kathmandu Research Institute for Biological Sciences, Lalitpurnews@myrepublica.com
More from Author
Without immediate action, there is real risk of the world turning to post-antibiotic order where treatable infections can kill many people
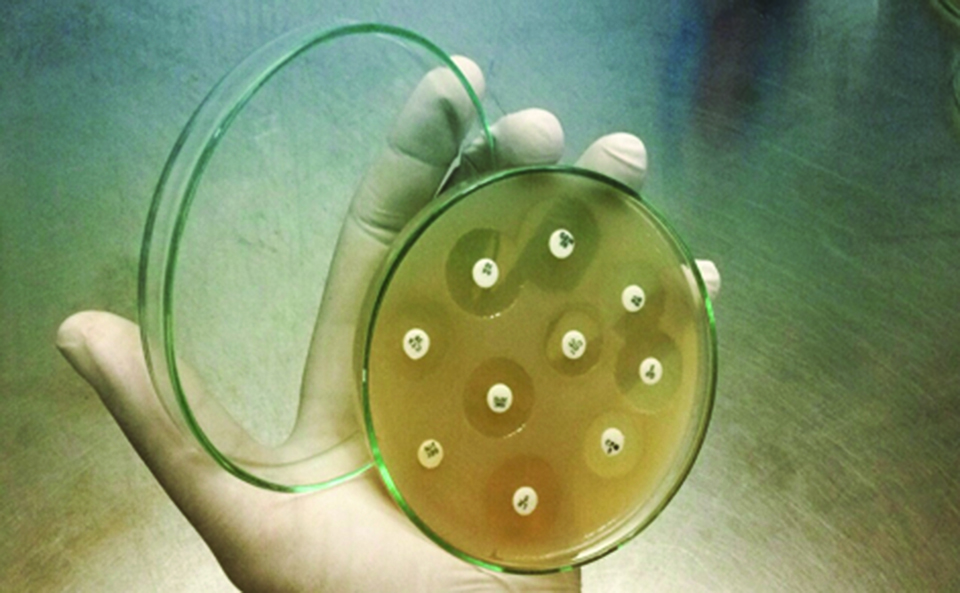
Antibiotics, crucial life-saving medicines, were ‘miracle drugs’ of the 20th century, but now they are not effective against pathogens to cure diseases. Antibiotic resistance bacteria also known as “superbugs” is now a global problem and can affect anyone, of any age, in any country. Last year we marked World Antibiotic Awareness Week (November 13-19) with the slogan ‘Seek advice from a qualified healthcare professional before taking antibiotics’. In Nepal, several awareness programs were organized with the slogan ‘think twice, seek advice’. Misuse and overuse in animals and humans enhances the process of antibiotic resistance. As a result, treatable infections become life threatening and more severe.
Globally, anti-microbial resistance (AMR) has become one of the biggest threats to the public health. On September 21, 2016, global leaders signed the UN proposal to stop the spread of infections that are resistant to antimicrobials. That was only the fourth time in the history of UN General Assembly where health topic had become the matter of concern in high level meeting. If anti-microbial resistance goes at the same speed, it will be responsible for killing nearly 10 million people annually worldwide by 2050— equivalent to one person dying every three seconds and more dying annually than from cancer.
The economic costs could be catastrophic: between $60 to $100 trillion. In Nepal, World Health Organization (WHO) has reported AMR as high as 69 percent among the bacterial pathogens. The leading causes of death include diarrheal diseases, lower respiratory tract infections and tuberculosis, urinary tract infections and sexually transmitted diseases caused by antibiotic resistant pathogens.
Ministry of Health and Population (MoHP) endorsed the antibiotic treatment guidelines designed to focus rational use of antibiotics throughout the country in 2014, but it has not been implemented effectively. AMR is worse in Nepal, India and other developing countries where practices of self-medication, availability of counterfeits drugs and inappropriate use of antibiotics have created an environment for drug-resistant microbes to flourish. In Nepal, AMR rate is alarming, but preparation to prevent future calamities is almost zero.
Use of antibiotics in livestock farming in our country is increasing day by day and is quite heavy compared to neighboring countries. Most drugs are used in animal farm to enhance growth rate. When we feed antibiotics as food supplement in animal farm, it helps the bacteria to develop resistivity to the same or similar drugs used during infection in human.
Additionally, most farmers purchase antibiotics from local retailers without veterinarian prescription. Data shows market of veterinary antibiotic in Nepal rose over 50 percent from 2008 to 2012. But no attention has been given to how antibiotics in livestock and agricultural farming contribute to rise of AMR. Antibiotic use in Nepali farm is increasing excessively though exact figure of amount and dose is not available. It has been found that the use of antibiotics in farm contributes to the development of resistant organisms which result in non-curable human infections.
Misuse and overuse of antimicrobial drugs in farming is one cardinal factor of antibiotic resistance. When we feed antibiotics to farm animals then the bacteria in and around the farm are exposed to the antibiotic, some of them die and others that drugs can’t kill survive, grow rapidly and later become a superbug. Then the superbug travels from farm to the kitchen via poultry or raw meats. Similarly, drug resistant strains can move to the surrounding environment via several routes. Thus antibiotics used in farm can create antibiotic resistant strain which is a looming risk to human health.
Since most farmers are illiterate they purchase the feed supplements for their livestock directly from the local market, but they are unaware of the presence of antibiotic growth promoters premixed in feed. Well trained veterinarians are scarce. Almost all the livestock food supplements are imported from India. Consumers are not aware about the fact that meat items infected with antibiotic-resistant bacteria could cause infection to them.
Need for action
Third National Summit of Health and Population Scientists in Nepal (April 10-12, 2017) had highlighted the need for formulation of evidence based guidelines to tackle AMR. This could be important to steer research in the race against drug resistant infection. Few months back WHO listed six pathogens as an antibiotic-resistant “priority pathogens, that pose the greatest risk to human health”.
The new strategy for novel antimicrobial should be disarming the pathogen. Scientists are turning different avenues to attack pathogens such as phage therapy (Bacteriophages, viruses that infect bacteria), use of antimicrobial peptides, screening essential oils and medicinal herbs for identifying new antimicrobial compounds, and development of vaccine against bacteria using bacterial membrane vesicles among others.
Effective antibiotic stewardship policy should be formulated to reduce spread of bugs. Prescribing antibiotic for treating viral disease must stop completely. Drug prescription must follow after antibiotic susceptibility test. There is an urgent need to search for novel therapeutic options because antibiotic resistant bacteria travel beyond the border. It is our responsibility to control them on time. Without immediate action, there is real risk of the world turning to post-antibiotic order where treatable infections can kill many people. We must work together to prevent the unnecessary use of antibiotics. This will help in controlling the spread of superbugs locally and globally.
Sherchan is Assistant Professor at Department of Global Environmental Health Sciences, School of Public Health and Tropical Medicine, Tulane University, New Orleans. Rayamajhee is Research Faculty, Department of Infectious Diseases, Kathmandu Research Institute for Biological Sciences, Lalitpur
sawmendra@gmail.com
rayamajheebinod@gmail.com
You May Like This

Jeremy Renner's wife says he once threatened to kill her, actor hits back
Amidst a bitter custody battle, Jeremy Renner's ex-wife Sonni Pacheco has claimed that the actor once threatened to kill her... Read More...

Leopard attacks kill 11 children in 5 years
ARGHAKHANCHI, Oct 4: An eight-year-old girl Prashanna Nepali of Sandhikhara Municipality-2 of Arghakhanchi district has been mauled to death by... Read More...

Militants storm army camp in Indian Kashmir, kill two
SRINAGAR, Nov 29: Militants attacked an army base near Jammu on Tuesday, killing two security personnel before taking positions inside the... Read More...






Just In
- CM Kandel requests Finance Minister Pun to put Karnali province in priority in upcoming budget
- Australia reduces TR visa age limit and duration as it implements stricter regulations for foreign students
- Govt aims to surpass Rs 10 trillion GDP mark in next five years
- Govt appoints 77 Liaison Officers for mountain climbing management for spring season
- EC decides to permit public vehicles to operate freely on day of by-election
- Fugitive arrested after 26 years
- Indian Potash Ltd secures contract to bring 30,000 tons of urea within 107 days
- CAN adds four players to squad for T20 series against West Indies 'A'











Leave A Comment