
OR
#MEMOIR
Surviving the Scourge: My Terrifying Encounter with COVID-19
Published On: July 20, 2023 03:15 PM NPT By: Dr. Kirti Kala Kharel

More from Author
Everything was normal. Every morning at 5 a.m., my phone's alarm reminded me that it was another day to get up and work, something I always liked doing. I prevented it from dozing and stayed in my dreams since "morning sleep" is inescapable. Finally, I woke up, weary of keeping it from buzzing again, and my day began with my normal ritual of making my bed, brushing my teeth, and taking a shower. My go-to meal was bread toast with avocado and an omelet, which kept me energized throughout the day. I reached my hospital around 9:30 a.m., well-prepared with my scrubs, white coat, and my stethoscope around my neck.
My day began with talking to patients, listening to them, writing down their medical history, and presenting the situation to the seniors and the team of medical specialists. They would then discuss the patients' health and treatment plans, making any necessary revisions to their care. The entire day, we would work together, and ultimately seeing any patient healthy and their grin when they were discharged would be the most satisfying and immense sensation of pleasure for me, making me delighted with what I was doing. That used to be my typical day at work.
One wonderful day, as we were talking and discussing various situations while eating lunch with our medical team, one of the physicians mentioned a report of a cluster of pneumonia patients in Wuhan, China, with a new coronavirus detected. The date was December 31, 2019. I assumed it was simply another virus at the time, but the coronavirus quickly spread all over the news, reaching other countries from China. After a month, on January 23, 2020, there was news of the first incidence of coronavirus in our country, Nepal, and this was the first time I became terrified and worried about the damage it may cause.
The small number of cases rose, and ultimately, on March 24, 2020, the government of Nepal enacted the first lockdown in history, which continued for another couple of months. It was a fearful scenario all around the world, and COVID-19 was already a pandemic. People stayed at home throughout the lockdown, while schools, transit, public areas, cinema halls, restaurants, marketplaces, and public and commercial offices were all shuttered. However, as healthcare providers, we doctors were on our duties, and hospitals were in demand. Now going to the hospital was different than before; everything changed from our usual scrubs to personal protective equipment (PPE). Wearing PPE was not easy. We struggled with sweating, fogging of goggles, spectacles, or face shields. And there was this dreadful scenario going on in the wards, limited beds for the COVID-19 patients.
The severe acute respiratory sickness induced by SARS-CoV-2 was dubbed COVID-19, yet the number of cases and deaths continued to rise in 2020. As the condition progressed, the number of such instances increased from 3-4 per day to 50-60 per day. Many of them would arrive with fever, cough, and minor shortness of breath, and we would send them home with appropriate symptomatic medications and advise them on precautionary measures. Another set of patients might "walk in" with fever, cough, and no evident shortness of breath. They would, however, have very low O2 saturation in their blood. Patients with "happy hypoxia" were referred to as such. This group of patients filled hospital beds, and every other day there was news about commercial/public facilities being converted into temporary hospitals to admit and treat an increasing number of cases. There would also be another set of individuals with severe symptoms who would require intensive care.
As a medical officer, I had to see numerous cases on an outpatient basis daily, and I also had a few assignments each week at the hospital ICU. And it was a different tale at the ICU. There were patients of various ages, including children, adults, and the elderly. This illness had taken no prisoners. On my first day in the ICU, I saw 10 COVID-19 patients. I prayed for a night free of major events, but it appeared that God had some other plan for us. At 11 p.m., I received a phone call. There was this 28-year-old dark, tall, cute but slender, scowled young boy with a worn face who was severely panting, coughing, and unable to stand. He appeared tired, worried, concerned, and seriously ill. He had been admitted to the ward for the past two days due to a fever and shortness of breath. I looked over his medical records and discovered that he had no history of medical difficulties. He did, however, have severe COVID-19 pneumonia.
His x-ray revealed several infiltrates on both sides. He was given steroids, antibiotics, antipyretics, and other pain relievers. There was no particular antiviral treatment available at the time. He merely required 2 liters of supplementary oxygen when he arrived, but his health deteriorated so much that he was sent to the ICU where he needed 15 liters of oxygen per minute. He appeared to be very unwell and was having trouble breathing, and ventilatory assistance was now his only hope of survival. Even with ventilatory assistance, he was unable to sustain oxygen levels. We increased his steroid dosages, modified his ventilatory settings for maximum support, tried everything possible we could, but his saturation remained low. Despite the greatest efforts of the ICU staff, he was sinking. He didn’t appear to see the light of day.
We summoned the family and explained the issues. It broke my heart to tell them that their kid was dying, and that we were unable to help. Parents of the patient were devastated by the news, and as their tears streamed down their faces, it looked as though they were slipping away from the earth. How on earth could they stand to accept that? We weren't prepared to deal with this scenario so soon either. They appeared to have lost their world. His mother was in a desperate state; she wailed, sobbed, and cursed God for stealing their only son. Their shattered faces still haunt me.
He left us a little over two hours later. I was shivering and powerless as I stood at his bedside, reflecting on the lethal nature of the illness and how lacking we are in armor in this battle against Corona. It broke my heart even more when his parents were not even permitted to touch their precious son's body since the condition was very contagious. The army was contacted, and the body was given to them in plastic bags. The government has made arrangements that soldiers perform separate funerals for those who passed away from COVID-19 with little or no family participation. I was praying for the wellness of the other nine COVID-19 cases while the troops removed his lifeless corpse.
And eventually, to see some of my own coworkers working at the hospital become infected with the virus and be in bed under masks, fighting for their lives, was a horrible situation and upsetting for me. When I thought about it, I had been extremely cautious, always adhering to corona safety guidelines, and maintaining physical (social) distance, but still, I got my COVID test positive. At first, I didn’t feel anything unusual, but after a few days, I started to feel unwell and became afraid. My situation deteriorated day by day. My entire body ached as if I had fallen from a lofty building, and every bone in my body hurt. Even a simple touch was full of tenderness. I can remember my chest was so heavy that it could possibly burst out. That pounding headache seemed like a thunderstorm brewing inside my skull. Despite my best efforts to cope with all of this, a sensation of loneliness stalked me as no near ones were permitted to see me while I was alone. I can’t tell you how much I missed being with them, holding them through that time. I used my phone to communicate with my family, and seeing their anxious faces would make me feel even more depressed. Checking my oxygen saturation level, taking antibiotics, and painkillers were a must to keep me getting better.
While I was suffering, I could identify with my many patients who had battled this sickness. I also lost my sense of smell. I attempted to smell something strong, like perfume, to see whether my nose was working, but I got nothing; there was no fragrance. I, too, had lost my appetite. For me, everything tasted the same. Nevertheless, I attempted to eat as much as I possibly could and kept myself motivated. After nearly fifteen days of isolation, care, and medicine, a glimmer of optimism arose when my body ache slowly vanished, and I felt gradually stronger and more invigorated than before. I began to feel much better. Suddenly, the world appeared to be lovely. My hunger gradually returned, and I could finally smell. My chest discomfort and cough have subsided. On the 24th day, I retook my COVID test, and thank God, it came out negative. I felt like I just won a major battle.
Today, as the days have stabilized and the fear of corona has subsided because of the effectiveness of vaccinations, people are returning to their daily routines, moving on from their sorrow and loss. Looking back, I sometimes marvel at how the world was rattled by a little virus. Our contemporary science and research, which we were so proud of, at one point became so weak and feeble, unable to help the COVID patient. And the big question remains, are we and our science capable of handling such difficulties if they arise in the future?
You May Like This
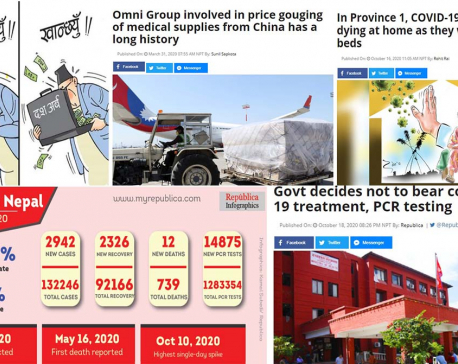
As Oli government limits its role to counting deaths during the greatest public health crisis, people are dying at an alarming rate
Experts say the government has decided to shred the constitution ... Read More...

India doctors ask for support as 196 die so far
NEW DELHI, Aug 9: The Indian Medical Association says 196 doctors have died of COVID-19 so far and, in an... Read More...

Udyapyur's District Hospital doctors on Dashain leave, patients deprived of treatment
GAIGHAT, UDAYAPUR Oct 1: Patients visiting the District Hospital Udaypur based in Bokse, looking for treatment have been deprived of the... Read More...



Just In
- Second day of Nepal Investment Summit to feature diverse discussions
- Ilam-2 by-election: UML’s Nembang leads by 4,523 votes
- UML’s Bhandari secures victory in Bajhang-1 by-election
- CIB probe into fake DL distribution case: PMO pressures public prosecutor to free arrested govt employees
- Police report one death in Bhojpur jeep accident
- Nepal faces Bangladesh Red in int'l U-19 Volleyball Championship final
- Nepal Investment Summit: Two organizations sign MoU for PPP cooperation
- Sita Air flight to Ramechhap returns to Kathmandu due to hydraulics issue















Leave A Comment