
OR
#COVID-19 and rural health infrastructure
Young doctors working at government hospitals outside Kathmandu sense a doomsday scenario
Published On: August 18, 2020 07:08 AM NPT By: Republica | @RepublicaNepal

KATHMANDU, Aug 18: Jharana Gurung is an ophthalmology student who is not yet a frontline professional to handle the COVID-19 cases. She will soon be joining on the frontlines of our battle against the virus, and she is nervous. She says she cannot even imagine wearing personal protective equipment (PPE), and handling patients in a chaotic situation.
"That is what comes to my mind when I think about the days ahead. The government has already told us to be prepared. I will probably be working at isolation centers soon as COVID-19 cases have spiked," said Gurung, who works at Lumbini Eye Hospital.
Earlier, around 1,000 patients would visit the hospital daily. As Nepal shut down international borders on march 24, the Indian nationals who used to come for treatments have stopped, and the daily visitor is around 300. Gurung says attending to those patients makes doctors vulnerable but 'that is being handled'. There are enough doctors in the hospital and there is no problem with PPE for now. "But we cannot say that the situation will be the same once we start attending COVID-19 patients," she anticipates.
The young doctor is not happy about the government preparations to fight the pandemic. She keeps on hearing of the lack of beds, ventilators and staff in hospitals in Province 5. "Sometimes this thought robs my sleep as well," she added.
Doctors like her want more isolation centers, quarantines and hospitals dedicated to COVID-19. Similarly, counseling and training to the health workforce were expected. "Better preparation and sensitivity from the government would make our fight against the virus robust."
Dr Arun Uprety, 26, has a similar take on the situation. The rising number of COVID-19 cases has left the medical officer at Charikot Hospital anxious, and the uncertainty about the future affects his mood. Not being able to see parents in Kathmandu for the last two and a half months, despite being stationed close by, has made him sad. "My father is a diabetic. My mother is a nurse. I keep worrying about them," he said.
Three older patients died in the hospital recently and the atmosphere at the facility then turned rather gloomy. They were not tested for COVID-19, but their life could have been saved if they could have been taken to a better hospital on time, wonders Uprety. According to him, it is not fair if other kinds of patients have to die simply because the government is busy dealing with the pandemic.
"COVID-19 seems to be the sole focus, and yet we are not well prepared. Here in Charikot, we have not expanded any physical infrastructure, nor any remarkable progress in terms of manpower, equipmenta," he reported, adding that the lack of trained force, enough space in hospitals and isolation wards are going to cost dearly in the near future.
"The money provided by the government barely covers the cost for critical patients, and private hospitals don't seem to be interested in joining the fight. There are lapses we need to revisit and address," he further said.
Nepal first registered the COVID-19 case back in January. After the second case was confirmed in March, the nation went into a lockdown. Essential supplies were procured, hospitals and health centers for COVID-19 patients were fixed, isolation wards and quarantines were run. But the influx of people coming from the southern borders and mismanagement that followed contributed in spreading the virus. On the other hand, returnees from other nations were also found to have flouted the pandemic guidelines. PCR testing of suspects and contact tracing of infected became challenging, and the situation worsened. Now, COVID-19 related deaths have crossed 104 while over 27,000 are infected. Patients with symptoms of COVID-19 are on the rise.
"We don't know what we are going to do if we start getting a huge number of patients with severe symptoms. In the past, there were only asymptomatic patients," said Anil KC, a doctor at Rolpa District Hospital.
KC stated that emergency cases should be referred to Dang or Butwal, as Rolpa is a very remote place to offer advanced facilities.
Earlier, it was not easy for KC and his team to gather courage to look after corona infected patients. Wearing a dress that covers the entire body part, visor, mask and gloves gave a chill. "The fear was deep, but we had no other way. Now, we are more used to it but we don’t know how we can handle symptomatic patients," he wondered.
Dr Surya Lama of BP Koirala Institute of Health and Sciences of Dharan talked about the pressure medical doctors go through when they have to take care of both their regular departments and pandemic cases. "We have to attend both our regular wards as well as the COVID-19 center. Though it's on a rotational basis, that's taxing," said the orthopedic doctor.
Citing the lack of beds and isolation wards in the periphery, a great number of COVID-19 infected have been visiting the hospital these days, according to Lama. "Even asymptomatic patients' inflow is huge," he noted.
The doctors told Republica that the tough work they do is not that rewarding, however. Biased treatment by the people in their neighborhood demotivates them. Unless their food and accommodation facilities are provided by the authorities, if health care personnel have to move out for even the essentials, they can easily be targeted by the community.
"We feel bad about such mistreatment, which is actually rampant. We got to be more humane and more understanding," said Lama.
As per the data of the Epidemiology and Disease Control Division, over 360 health professionals across the country have been infected by COVID-19 so far. Ine view of the deepening pandemic, the government has directed the entire medical fraternity to be ready for action.
You May Like This
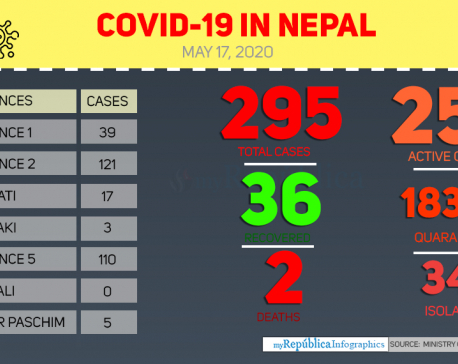
Health ministry confirms three new COVID-19 cases, number of total cases reaches 295
KATHMANDU, May 17: Nepal reported three new cases of COVID-19 on Sunday evening, taking the national tally to 295. ... Read More...
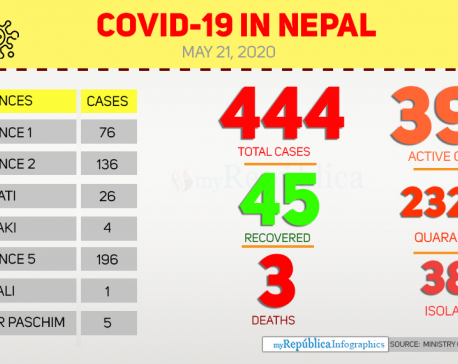
Nepal reports third COVID-19 death; Gulmi patient dies today
BUTWAL, May 21: Nepal has reported the third death due to COVID-19. A 41-year-old male patient from Madane Rural Municipality-6,... Read More...
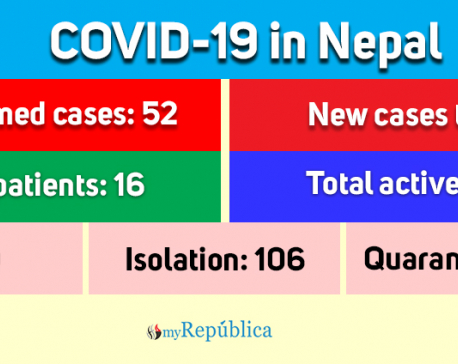
Government allows private labs to conduct COVID-19 tests
KATHMANDU, April 27: Government has made ways out to conduct lab tests for novel coronavirus disease from private labs also. Read More...





Just In
- Illam by-election: Nepal-India border to be 'sealed' from midnight today
- Gold price rises by Rs 500 per tola
- Emir of Qatar returns home after wrapping up state visit to Nepal
- Senate passes bill forcing TikTok’s parent company to sell or face ban, sends to Biden for signature
- PM Dahal hosts luncheon in honor of Qatari Emir
- Tata Sumo accident in Kavre leaves 10 injured, three in critical condition
- West Indies ‘A’ cricket team arrives in Nepal
- Barpark commemorates 2015's Gorkha Earthquake



_20240423174443.jpg)







Leave A Comment