
OR
Understanding COVID-19: Dos and Don’ts
Published On: May 19, 2021 12:23 PM NPT By: Dr Prakash Budhathoky

Dr Prakash Budhathoky
The author is a treasurer at Central Executive Committee of Nepal Medical Associationnews@myrepublica.com
If the patient is given steroid (dexamethasone)/LMWH/antiviral at the onset of pneumonia (Day 3), mortality should be an exception and not a rule.
It’s been 17 months since COVID-19 was first detected in December 2019 in Wuhan, China. We have come a long way since then and the knowledge and experience gained over this period of time has certainly helped to better manage the patients. Diagnosis and treatment on time give the patient the best chance to recover from COVID-19. It is important to carefully elicit medical history. It is crucial to know what should be done and what should not be done in the given clinical situation.
Atypical minor symptoms
The symptoms of COVID-19 are no longer limited to the respiratory system (dry cough, fever, and difficulty in breathing). Many extra-pulmonary symptoms of COVID-19 have now been reported. These may differ even in different members of the same family.
Several atypical symptoms of COVID-19 have been reported. These include: nausea/vomiting, diarrhea, headache, increased frequency of urination, right abdominal pain, sudden loss of taste and/or smell (bitter and sour tastes are retained), oral and skin lesions (rash, vesicles), conjunctivitis, COVID-toes (presenting as gout-like symptoms), hiccups, calf pain, tiredness, malaise, dizziness, etc. Such unusual symptoms of COVID-19 are likely to be missed. Do think of COVID-19 in these times and get the patient tested.
Isolated diarrhea
Diarrhea may sometimes be the only symptom of COVID-19. Later on fever, cough may or may not develop. Acute diarrhea in COVID-19 is always small intestinal diarrhea. It is painless, there is no blood or mucus in the stool. The virus may remain in the stool for up to 3 months. A patient who has diarrhea may be a super—spreader. If a patient presents with a new-onset of intermittent diarrhea for 48 hours duration, the risk of COVID-19 infection is high.
Fever
Fever of COVID-19 is typically low grade - less than 100.4 degree Fahrenheit - and occurs after exertion. The fever is inflammatory and not due to the viral infection. It does not respond to paracetamol, instead the fever responds to anti-inflammatory drugs like mefenamic acid, naproxen, nimesulide and indomethacin. Do not miss first-time detected, low grade fever after exertion. This may often be the first symptom of COVID-19.
Day 1 of illness
A person can test positive for COVID-19 even when there is a single symptom. This can be single loose motion, headache, loss of smell, calf pain, isolated skin rash and any other non-specific symptom as discussed above. Other symptoms may appear after 48-72 hours.
If you have been exposed to COVID-19, the first symptom is most important. Do not ignore any symptom which cannot be explained. This is Day 1 of the illness - the test may or may not be positive. Day 1 is important as pneumonia usually will develop around Day 3 of the infection.
Day 3-6 of the illness
Critical days are Days 3-6 after the first symptom or positive test, whichever is earlier. The patient may develop pneumonia around the third day of the illness, although not every patient develops pneumonia. Look for fall in SpO2 on 6MWT by 4 (hypoxia; this may be a sign of micro-or macrovascular emboli) or development of exertional tachycardia or difficulty in talking or cough; these are suggestive of pneumonia. If undetected and untreated, complications may set in after Day 5.
If the patient is given steroid (dexamethasone)/LMWH/antiviral at the onset of pneumonia (Day 3), mortality should be an exception and not a rule.
Recognizing red flags
Not taking due precautions for any comorbid condition, fall in SpO2 or development of shortness of breath or cough on 6Minute Walk Test, CRP >26, absent eosinophils and absolute lymphocyte count <1000 on CBC are red flag signs of COVID-19.
Do baseline CBC, ESR, CRP, CRT, ferritin and/or D-dimer. Repeat ESR, CBC and CRP daily. Do not ignore isolated lymphopenia and eosinopenia on Day 1 of the illness. These may sometimes predate inflammation and may be a sign of oncoming inflammation.
Treat the patient not report
The RT PCR test using throat/nasal swab is the gold standard test for the diagnosis of COVID-19. But it has a sensitivity of around 67%. This means that about 33% of the results may be positive but the result comes negative-false negative. Rapid antigen tests may also give false negative results.
If the patient has classical symptoms of COVID-19 and the report is negative, repeat the test. A CT scan or chest X-ray can be done on Day 1 itself. If you suspect that the patient has COVID-19, don’t wait for the confirmation.You may miss Day 3 of the illness, so then you will miss pneumonia, happy hypoxia. So, isolate the patient and start treatment.
Therefore, always interpret the test results with the clinical presentation of the patient.
Mistaken as typhoid
If you miss COVID-19, thinking it to be a case of typhoid fever, that can be dangerous. If you miss COVID-19, you will miss pneumonia on Day 3-6 and complications can develop, which may be irretrievable at times. Unless the blood culture is positive, do not treat these patients for typhoid.
Gargling
Evidence has shown that the virus is present in high quantities in the throat, making it a major reservoir of the virus in both Symptomatic and asymptomatic ones. Although gargling will not eliminate the virus, it reduces viral load in throat thereby reducing risk of transmission.
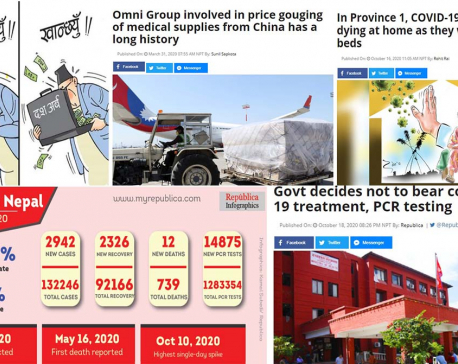
Now, the local administration in 73 out of the 77 districts has enforced prohibitory orders in order to prevent and break the chain of transmission of the virus. Although the prohibitory orders have had a negative impact on the economy, education along with social and psychological consequences is necessary. The second wave is mainly due to newer, more contagious variants known as B.1.617, B.1.1.7, and thus resulting in rapid transmission. And, surprisingly, shortness of breath is the most common clinical feature among symptomatic patients in the second wave needing very high supplemental oxygen. Therefore, apply public health measures. Prevention is better than cure.
(The writer is Treasurer at Central Nepal Medical Association)
You May Like This
As Oli government limits its role to counting deaths during the greatest public health crisis, people are dying at an alarming rate
Experts say the government has decided to shred the constitution ... Read More...

VIDEO: Diplomacy in the time of coronavirus: Johnson and Macron trade bows, thumbs up
LONDON, June 19: Standing apart on either side of a strip of red carpet outside Number 10 Downing Street, Prime Minister... Read More...

India’s virus caseload now 4th highest in world
NEW DELHI, June 12: India’s coronavirus caseload has become the fourth-highest in the world, overtaking Britain, by adding 10,956 new... Read More...

Just In
- World Malaria Day: Foreign returnees more susceptible to the vector-borne disease
- MoEST seeks EC’s help in identifying teachers linked to political parties
- 70 community and national forests affected by fire in Parbat till Wednesday
- NEPSE loses 3.24 points, while daily turnover inclines to Rs 2.36 billion
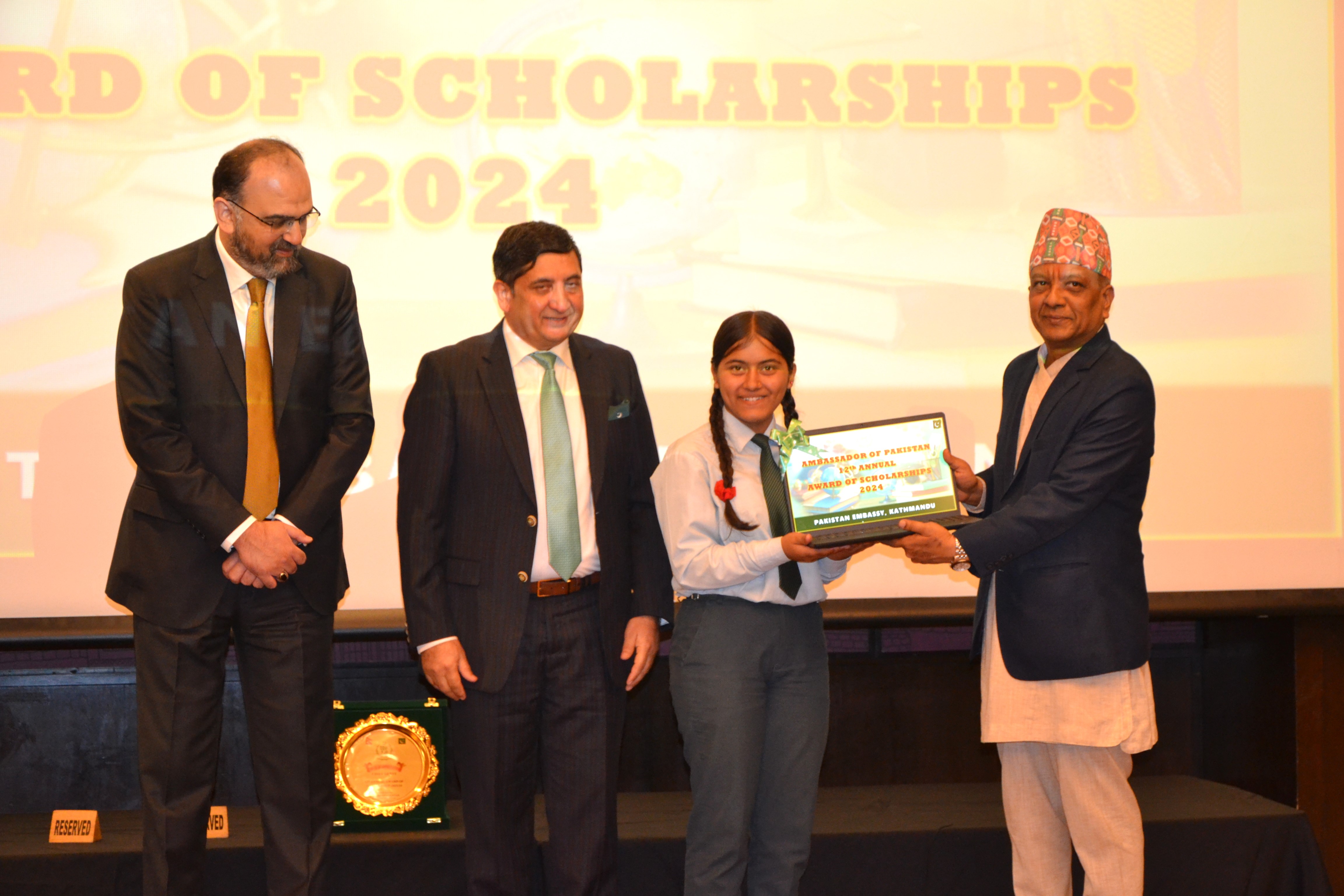
- Pak Embassy awards scholarships to 180 Nepali students
- President Paudel approves mobilization of army personnel for by-elections security
- Bhajang and Ilam by-elections: 69 polling stations classified as ‘highly sensitive’
- Karnali CM Kandel secures vote of confidence














Leave A Comment