
OR
Positive PCR results in patients recovered from COVID-19 may not be reinfection
Published On: May 13, 2020 10:24 AM NPT By: Dr Rojeet Shrestha and Dr Puja Neopane

Dr Rojeet Shrestha and Dr Puja Neopane
Shrestha is an assistant professor at Hokkaido University, Japan. Twitter: @Rojeetshrestha Neopane is a microbiologist at Hokkaido University, Japannews@myrepublica.com
Nepal recently reported three cases, who are believed to be recovered from the novel coronavirus infection (COVID-19), being tested positive for the virus again. According to the Ministry of Health and Population, a 54-year-old man from Kathmandu, who was discharged from hospital on April 26, tested positive for the virus again. Similarly, a 44-year-old man from Parsa and a 19-year-old teenager from Rautahat were declared recovered and discharged on April 29 after three consecutive negative reports of PCR test. Both of them later tested positive for the virus during a follow-up investigation.
Other countries have also reported similar incidence, raising alarm that the virus might be capable of reinfecting the recovered patients. Japan is the first country to report a case of the positive virus test in recovered patients again. A few weeks earlier, South Korea reported that over 260 clinically recovered patients with negative virus test results later tested positive when retested after subsequent days. Data from Wuhan, China (where the outbreak emerged) shows that about 5 to 10 percent of the recovered COVID-19 patients tested positive for the virus , raising speculation that patients once recovered could become reinfected.
We will be discussing various factors that can lead to positive virus tests in recovered patients. Before that, it is necessary to understand some fundamental principles behind virus testing in the laboratory and our immune response against this novel coronavirus (SAR-CoV-2).
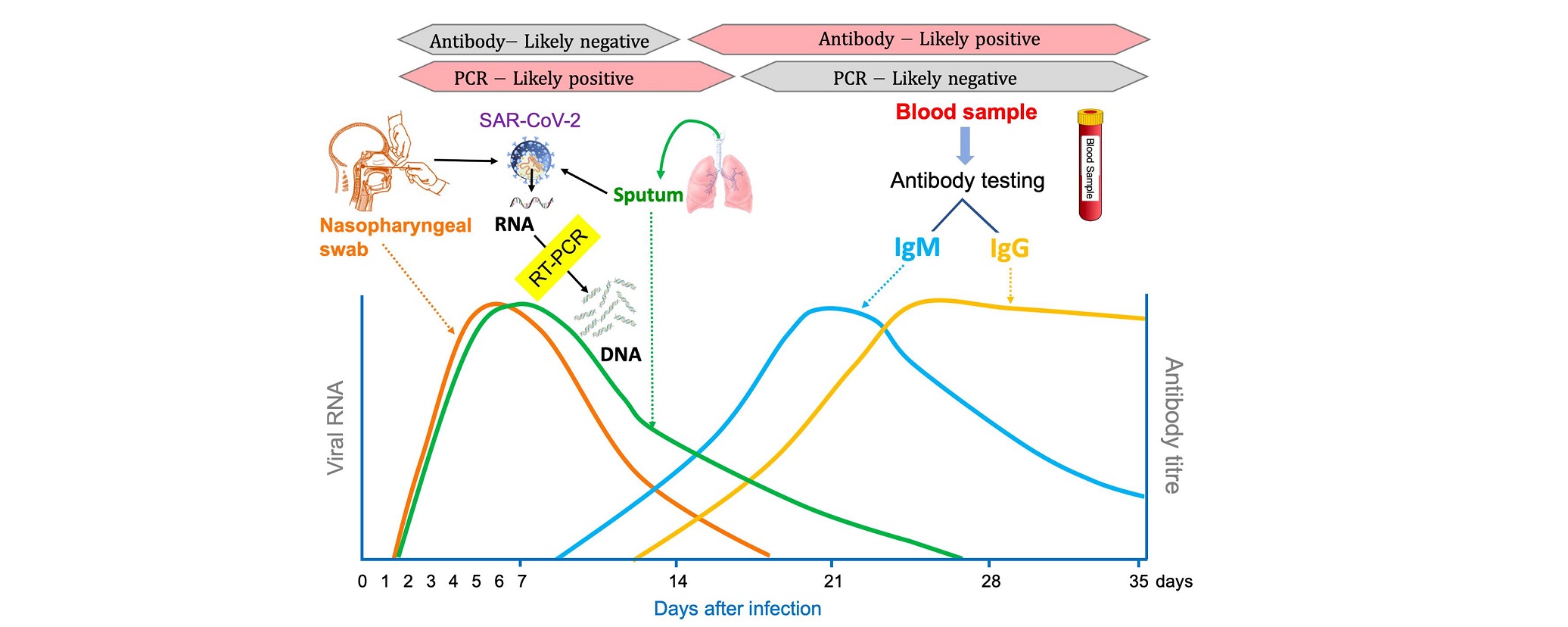
Polymerase chain reaction (PCR) is a gold standard test used worldwide for the diagnosis of COVID-19. PCR is a laboratory tool to identify a specific segment of the DNA in the sample. In this technique, a target DNA in the sample is amplified to millions of copies allowing for its easy detection. The coronavirus is ribonucleic acid (RNA) virus (it does not contain DNA). Therefore, it is necessary to convert RNA from the virus into its complementary DNA (cDNA) sequence using reverse transcriptase. Hence, this test is also called reverse transcription PCR (RT-PCR). As this virus can multiply its number in the cells of the respiratory system, specimens taken from the respiratory tract are ideal for its detection. Specimens collected from the upper respiratory tract like nasopharyngeal swab is common in practice while lower respiratory specimens like sputum and bronchoalveolar lavage (BAL) can yield more viral recovery. The peak of viral shedding appears in 3-5 days after infection. So this is the preferred time for the collection of specimens. RNA is isolated from the samples and converted into cDNA followed by its amplification into millions of copies using PCR. Detection of the unique sequence of RNA fragments of the coronavirus is diagnostic and this test can be used to diagnose COVID-19 in its early-stage when patients are highly infective. It is the most commonly used and reliable test to diagnose COVID-19. However, it is important to note that a positive PCR test means the sample contains RNA of this virus. It does not indicate that the virus is alive (active) in the sample. To confirm if the virus in the sample is viable, virus culture should be done. The viral culture facility is currently not available in Nepal.
When the coronavirus enters our body, it stimulates the immune system to fight against this infection. One way of the defense system is to produce antibodies that can destroy the virus. Usually, patients start producing IgM type of antibody within 8-10 days of infection. It will reach a peak in about a month of the infection and then slowly declines (see picture). The patient also produces another type of antibody called IgG, which starts to rise in blood within 10 - 12 days of infection and remains in the blood for a long time, at least several months. As the level of these antibodies increases in our body, it neutralizes the virus, and the patients slowly recover from the disease. Therefore, in most cases, the number of active viruses disappear by the third week of infection.
So what causes positive PCR results in recovered COVID-19? There are basically four reasons for positive PCR results in the recovered patients.
1. Testing errors (incorrect report)
"False-negative" results are not uncommon in PCR testing. It is important to confirm that the "negative report" is truly negative. If the PCR test that is performed before discharging a patient is "false-negative" because of flaws in the testing process and PCR results get positive during follow-up of patients after recovery, it is not appropriate to say the person has been "reinfected". Several reasons can cause false-negative results, including flaws in chemicals and methods used in PCR, inappropriate specimen collection, type of specimen used, inappropriate storage and transportation of the samples. Most often the false-negative results are due to a poor quality specimen (not a deep nasopharyngeal swab) or the virus was at a very low number when the swabs were collected. Furthermore, the timeline of PCR positivity is also different in the types of specimens used. PCR positivity declines more slowly in samples from the lower respiratory tract like sputum compared to upper respiratory tract samples like nasopharyngeal swabs (see picture). Therefore, it is possible to get negative PCR results from nasopharyngeal swabs and positive from sputum during the recovery phase. Hence, the WHO guidelines on clinical management recommended that a clinically recovered COVID-19 patient should test negative for the virus twice, with tests conducted at least 24 hours apart, before being discharged from the hospital.
2. Re-infection
There is no enough evidence to ensure that patients once recovered from the virus can not get reinfected. However, considering the timeline of PCR "re-positivity" and the prevalence of the disease in our community, it is extremely unlikely that these patients are re-infected. More importantly, most people who are infected from the virus develop antibodies and other cellular defense mechanisms that can fight off the virus if they encounter it again. As shown in the picture, within 1-2 weeks of infection, our body produces antibodies against the coronavirus which remains in the blood for at least several months making them at least temporarily immune to the virus. For some viruses like measles, such immunity lasts lifelong. For other coronaviruses such as SARS, studies showed that the immunity can last from a few months to a couple of years. To this date, no human reinfection of this novel coronavirus disease has been confirmed and there is no evidence that a person who tested positive for the virus after recovery can transmit the disease to other people. A study published in Journal of American Medical Association (JAMA) published on May 11, 2020 suggested that recovery from COVID-19 might confer immunity against reinfection, at least temporarily.
This coronavirus is new and we do not have enough evidence to certainly know how long such antibodies remain in our blood to protect us from re-infection. However, follow-up tests in Nepal were conducted within a "relatively short time" after the patients were declared recovered, so it is unlikely that they were re-infected. Therefore, the use of the term "re-infection" should be cautiously used as it may be misleading.
3. Re-activation
Re-activation of the virus could be another reason for PCR to turn positive again in the recovered patients. In most cases, our immune system is able to destroy the viruses completely. However, in some people, the virus may remain inactive for a certain time and remains hidden from our immune cells. When the viruses are in this latent state, it does not cause any illness. However, these inactive viruses may get reactivated again and multiply its number, causing illness.
This type of phenomenon is common in certain viruses. For instance, the chickenpox virus in some patients may remain hidden from the immune system for a long time and get "reactivated" when the person's immune system is weakened causing varicella-zoster (Herpes-zoster). If the coronavirus could act in the same way, the person already has some level of immunity against the virus so the symptoms of the disease will be generally milder and self-limiting. So even if there is a chance of re-positive results in PCR after re-activation, such individuals have a low risk of infectivity.
It may also be possible that the virus might have never been completely cleared off in such patients. Instead, the virus might have been still active in tissues other than respiratory systems while patients were declared recovered based on the PCR report from the nasopharyngeal swab. Therefore, it might be necessary to test samples like stool and urine before declaring recovered. Many scientists believe that reactivation could be one of the plausible reasons for turning the PCR test back to positive in patients who have recovered. Further studies are needed to explore the possibilities of re-activation.
4. Detection of Dead viral fragments
This is the most important cause that can lead to positive PCR results in recovered patients. During the recovery phase, the virus is killed by our immune system but the dead viral particle may remain in the cells for several weeks after recovery. As the cells in the lungs heal, the dead cells containing viral particles are desquamated and coughed up into the throat, from where samples are taken. Since these dead viral particles contain RNA fragments of the virus, it can be detected by PCR resulting in "false-positive" results. According to Dr. Maria Van Kerhhove, technical lead of WHO's Health Emergencies Program, "in those people who tested negative after recovery and tested positive again after several weeks is due to dead lung cells which are coming up. It's not an infectious virus, it's not reactivation but it's actually part of the healing process". Furthermore, a report from Korea Centers for Disease Control and Prevention (KCDC) states that they were unable to isolate live virus from the sample of individuals who have recovered but again demonstrated positive PCR indicating that tests in these recovered patients are more likely to be "false-positive". KCDC emphasized that such individuals have little or no contagiousness. Therefore, patients who are declared recovered and later tested positive for PCR tests are still expelling dead lung cells rather than getting a new infection.
It is very crucial to understand that PCR is a test to detect the RNA of the virus but not the live virus itself. In other words, a “positive PCR" result reflects only the detection of viral RNA and does not necessarily indicate the presence of viable viruses itself. Therefore, recovered patients who tested positive again are less likely to be reinfected. Instead, the test is false-positive because of the presence of dead viral fragments in the samples. Viral culture should be performed from these specimens in order to rule out if it is the case of reinfection or reactivation.
So, PCR is a test to detect RNA of the virus but not for the active (live) virus. People who have recovered from coronavirus infection are less likely to get re-infected within a few months. The most common cause of turning PCR results back to positive in recovered patients is due to the presence of dead viral fragments.
Shrestha is an assistant professor at Hokkaido University, Japan. Twitter: @Rojeetshrestha
Neopane is a microbiologist at Hokkaido University, Japan
You May Like This
Nepal’s COVID-19 case tally nears 250,000
Nepal sees 821 new COVID-19 cases, 842 recoveries on Monday ... Read More...

Biratnagar sees yet another coronavirus-related death
BIRATNAGAR, Oct 2: Biratnagar reported yet another coronavirus-related death on Friday. ... Read More...

Minister of Internal Affairs of Province 2 Gyanendra Yadav tests positive for COVID-19
JANAKURDHAM, Aug 6: Minister of Internal Affairs and Law of Province 2 Gyanendra Yadav has tested positive for coronavirus. ... Read More...



Just In
- Bhajang and Ilam by-elections: 69 polling stations classified as ‘highly sensitive’
- Karnali CM Kandel secures vote of confidence
- National Youth Scientists Conference to be organized in Surkhet
- Rautahat traders call for extended night market hours amid summer heat
- Resignation of JSP minister rejected in Lumbini province
- Russia warns NATO nuclear facilities in Poland could become military target
- 16th Five Year Plan: Govt unveils 40 goals for prosperity (with full list)
- SC hearing on fake Bhutanese refugees case involving ex-deputy PM Rayamajhi today













Leave A Comment