
OR

More from Author
Doctors are paid poorly. They do not get housing and transport perks and even salaries are, at times, delayed or unpaid for months
We’re all concerned about the economy. We’re all eager to see our political leaders solve the problem of unemployment. But little is talked about the problems MBBS graduates and doctors face in this country. Here follows the same.
The MBBS training does not prepare students for their service in rural Nepal. Though students are required to spend time in communities, the training is not adequate to enable them to work independently in rural areas, handle administrative responsibilities, interact with rural communities, and live in rural Nepal. Now some institutions have carefully designed curriculum to prepare students for practice in rural Nepal and it would be interesting to follow the progress on it. But many self-financing students have their goals set firmly on examinations like the United States Medical Licensing Examination, UK Professional and Linguistic Assessment Board and postgraduate entrance examinations and/or establishing an urban practice.
A similar situation may exist in medical schools in other south Asian countries and other developing nations. Most private schools in South Asia are set up as for-profit enterprises, and investment and resources are likely to be channeled to areas which provide maximum returns. There is a need to train doctors who are skilled in communication, who have compassion for their patients, who are also required to be excellent rational clinicians able to respond to emergency situations. There is also the need for doctors to be competent not just in individual clinical care but also in community care.
Lacking in knowledge
An MBBS doctor fresh after MBBS supposedly knows modern scientific medicine and its branches to the extent taught and experience gained during four and half years of study and one year of internship training he receives. Following this he is expected to learn skills essential to practice of medicine. Ministry of Health and NMC-Code of Ethics and Professional Conducts (2017) have emasculated the MBBS degree to an extent that except for routine fever or diarrhoea the MBBS generalist has nothing to do professionally. Despite being a Bachelor of Medicine, Surgery and Obstetrics and Gynae an MBBS cannot gain proficiency in any one. Unfortunately there is no document which defines the complete scope of work that an MBBS doctor can do. The super specialist culture deeply prevalent in Nepal today encourages treatment of organs rather than of the human body. The role of MBBS in clinical practice has been gradually but surely emasculated to the level that a catheterization is to be done by a urologist and an ECG by a cardiologist. In this environment, role of MBBS in clinical practice today is demoted to that of a glorified clerk and phlebotomist.
Doctors without jobs
Nepal produces 2000 MBBS graduates every year and 500 foreign medical graduates come to Nepal every year. Even if only around 40 percent clear the Foreign Medical Graduate exam that still makes the number of qualified and licensed MBBS doctors produced yearly at 2000.
The government which is the largest employer has 60 vacancies every year for MBBS doctors to work in government hospital. About similar number is employed yearly by various government agencies like police, army and other institutions. This leaves around 2400 newly graduated MBBS doctors looking for jobs every year.
MBBS doctors today are threatened, victimized, and beaten up and hauled up to hospital administration. And senior specialist doctors are harassed by various officials under various acts and laws. This despite the fact that our work is the noblest of all and our intention is always good. Government does not give any encouragement or subsidy to health sector. Nearly 80 percent of healthcare of this nation is in hands of small private clinics and nursing homes which do their job unprofessionally. Lopsided policies of the government favor corporate healthcare instead.
Medical education has been taken over by unscrupulous businessmen in partnership with our politicians. MBBS doctors today are unemployed and underpaid. Difficult working conditions, lack of support from other specialties and hospital administrators, as well as rising healthcare costs have all slowed the development of MBBs doctor in Nepal.
While it is well recognized that the ability to provide care to acutely ill patients is essential to any healthcare system, Nepal needs to strengthen its emergency care through standardization of MBBS training and continuing medical education.
Joining a government service these days is being gradually made impossible for all doctors who are made subservient to multiple masters. They are paid poorly, do not get any of the perks like housing, transport and security and even the salaries are, at times, delayed or unpaid for months. Despite this they cannot go on strike or protest. We fight against ignorance, misconceptions, misdirected faith, and various taboos to inculcate scientific knowledge and impart health literacy among the public only to be targeted for doing our job.
According to the Nepal Medical Council, total registered medical doctors are around 24000 (18000 MBBS and 6000 specialist doctors). MBBS doctors annually produced in Nepal and abroad range from 1,500 to 2,000. Total vacancies for MBBS doctors stand at 1650 in Nepal’s government hospitals. Only 700 posts have been fulfilled, remaining 950 posts remain unfulfilled.
Rural areas of Nepal have one doctor for every 150 000 people, compared to one for every 850 people in Kathmandu Valley. The state of health care in Nepal is abysmal. Millions of Nepalis do not have reasonable access to adequate health services. The disparity in health status between urban and rural populations is particularly shocking. Many of the rural government hospitals lack basic equipment and some have not been staffed for years.
Let us not deny the fact that the country needs more qualified doctors—not just ‘doctors’—of modern scientific medicine. We already have surplus of persons masquerading as doctors of modern scientific medicine without adequate knowledge. If we get more qualified ones they can make a difference in Nepal’s health service system.
The author is a medical doctor
Twitter: @prbanjade
You May Like This

Doctors and development
Some doctors are not sympathetic to their patients. They launch their stethoscopes at private clinics and hospitals against their patients... Read More...

Path of peril
Even though politics of here and now demands repositioning of Nepali Congress, playing to the religious gallery might prove to... Read More...
Tap the opportunities
Low level of economic integration combined with untenable trade deficit is making Nepal vulnerable to external shocks ... Read More...



Just In
- World Malaria Day: Foreign returnees more susceptible to the vector-borne disease
- MoEST seeks EC’s help in identifying teachers linked to political parties
- 70 community and national forests affected by fire in Parbat till Wednesday
- NEPSE loses 3.24 points, while daily turnover inclines to Rs 2.36 billion
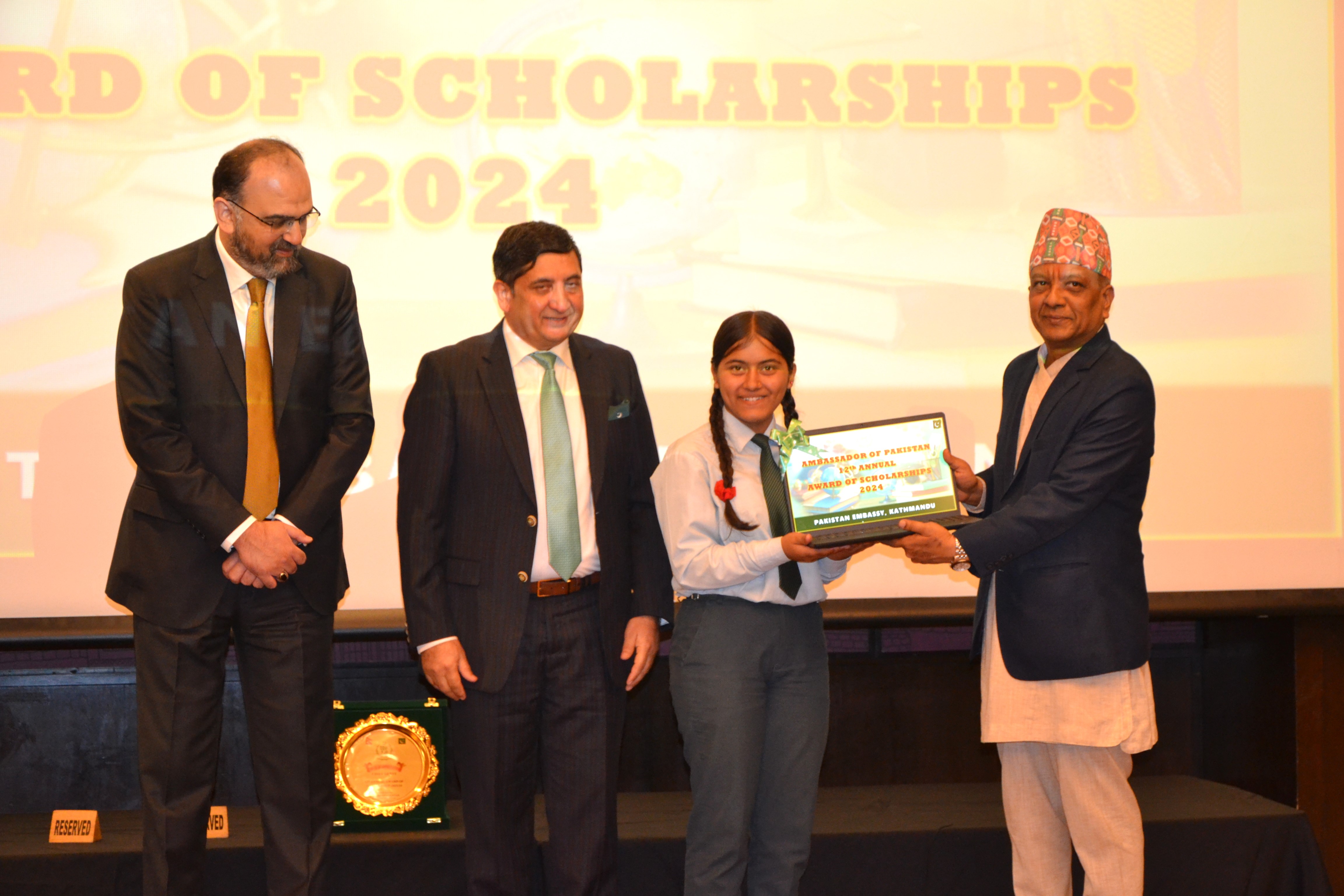
- Pak Embassy awards scholarships to 180 Nepali students
- President Paudel approves mobilization of army personnel for by-elections security
- Bhajang and Ilam by-elections: 69 polling stations classified as ‘highly sensitive’
- Karnali CM Kandel secures vote of confidence













Leave A Comment