
OR
More from Author
Climate change is becoming a cardinal cause for high number of dengue cases in several parts of the country
Dengue, also nicknamed breakbone fever and now emerging as a serious public health threat to Nepal, is a viral disease caused by virus belonging to Flaviviridae family closely related to four different serotypes—DEN-1, DEN-2, DEN-3 and DEN-4. That’s why an individual can be infected with a dengue virus as many as four times in her or his lifetime.
Dengue virus spreads from a person to person through the bite of an infected Aedes species mosquito. The same mosquito is a vector for transmitting yellow fever, chikungunya and Zika infection. It breeds on clean water and is responsible for Dengue fever (DF) and more severe and fatal forms like Dengue Hemohargic Fever (DHF), and Dengue Shock Syndrome (DSS). Dengue is common in more than 100 countries of our planet. Nearly 40 percent of the world’s population lives in dengue-risk areas.
In Nepal, dengue was first reported in 2004 from Chitwan and multiple outbreaks have been reported since then. The year 2016 was characterized by massive dengue outbreaks worldwide whereas the significant reduction was seen in 2017. But climate change is poised to increase the spread of deadly mosquito-borne disease in 2019, which is being common in several parts of the world with warmer climates like India, Brazil, coastal areas of China and Japan, and inland regions of Australia. Climate change is becoming a cardinal cause for high number of dengue cases in several parts of the country.
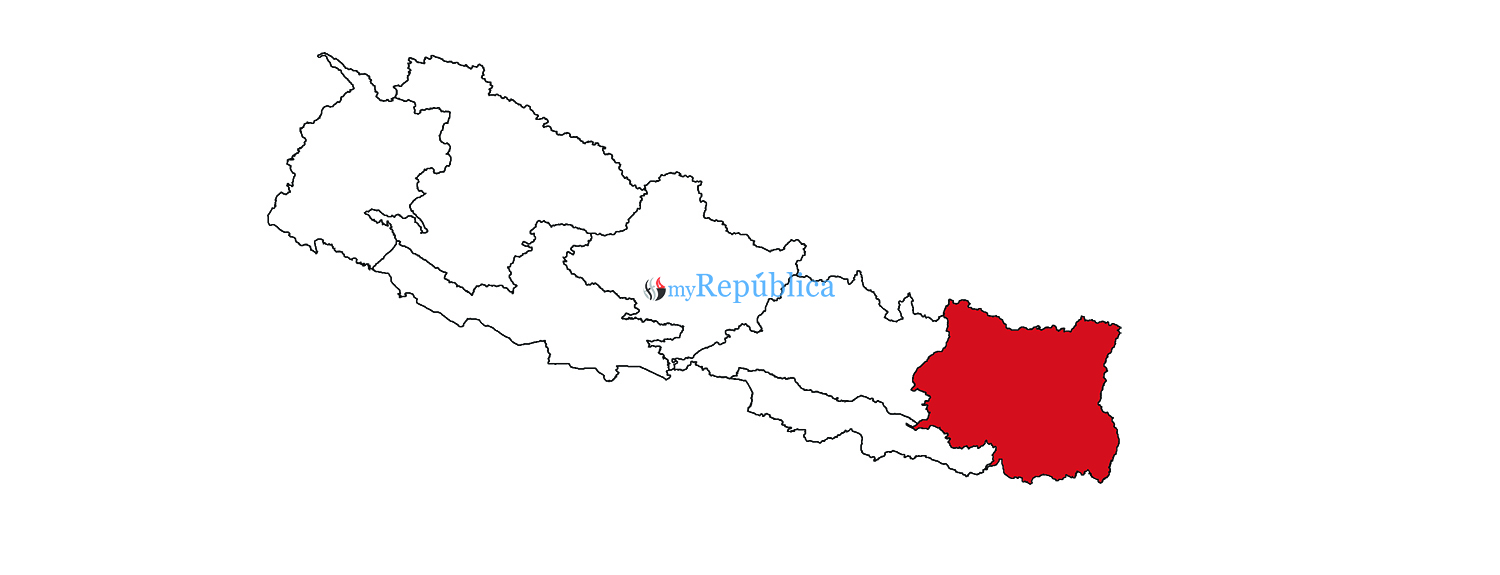
After dengue outbreak in Dharan, cases are being reported from more than 40 districts including Kathmandu where above 55 cases have reported by August 22. Dengue has started to spread even in hilly districts like Rukum, Dailekh, Achham, Panchthar and Kalikot. This year dengue cases were first detected in Damak and since then hundreds of patients have been found in different parts of the country. More than 5,000 dengue cases have been reported from Dharan alone and it is increasing day by day.
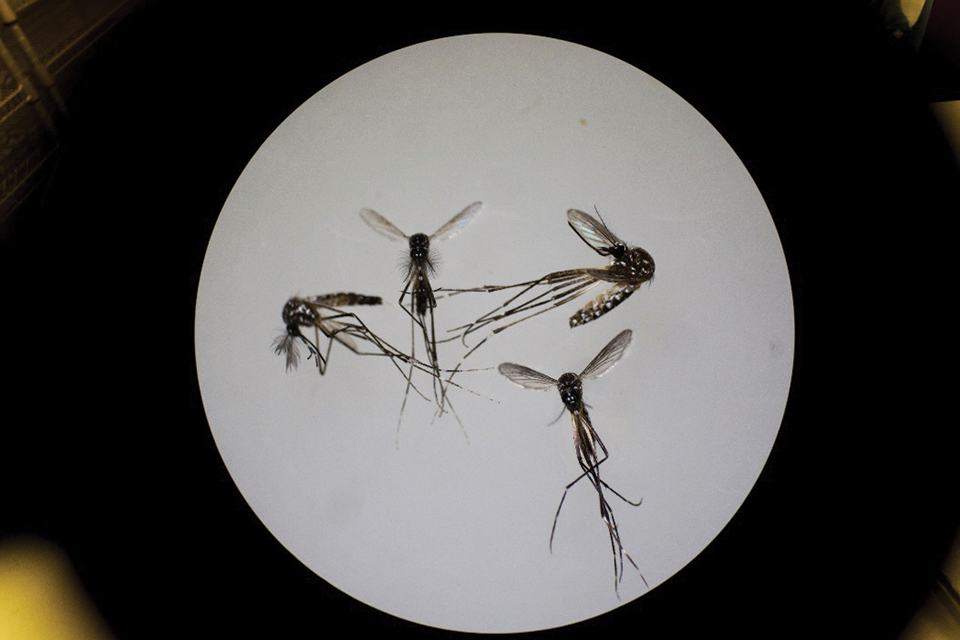
Transmission of dengue occurs by the bite of female mosquito belonging to genus Aedes and its two species, Aedesagypti being a primary vector and A. albopictus a secondary vector. In Nepal, A.albopictus also called as Asian tiger mosquito is the major vector responsible for transmission of dengue this year. A. agypti was a major vector last year. A. albopictus is highly adaptive and can tolerate freezing and sustain in many different microhabitats. These mosquitoes are recognized by white and dark markings on its legs. They thrive in stagnant water including puddles, discarded tires, pottery vessels, beer cans, and several other man-made containers and basically lay eggs near standing water containers. Uncovered water tanks and discarded plastic cups/tires have become the breeding sites for dengue-carrying mosquitoes. Interestingly, these mosquitoes prefer to live near people. Mosquitoes can get infected when they bite an infected person with dengue virus and then can transmit it to healthy people. It is also reported that an infected pregnant woman can transmit the virus to fetus during pregnancy.
The most common symptom of dengue infection is high fever, which may be accompanied by vomiting, nausea, joint and muscle pain, severe headache, pain behind the eyeballs, and skin rash. Basically symptoms last for two to seven days. Some cases are even asymptomatic. Nearly one in 20 patients infected with dengue virus will develop severe form of dengue which is a medical emergency. Severe form of dengue can cause internal bleeding, shock, and even death of the patients. People with low immune system like pregnant women, infants, and elderly people are at higher risk. Some of the warning symptoms of severe dengue are bleeding from the gums or nose, blood in stool, stomach pain, tenderness, vomiting and restlessness. Severe dengue requires immediate medical treatment.
Prevention is the key
Recent travel history and past medical history of patients should be examined to identify whether the infection is due to dengue virus. After onset of dengue symptoms, Dengue Virus Antigen Detection (NS1) test is done using serum sample of patients, which is a rapid diagnostic test. Additionally, serological tests like Dengue virus-specific IgMAntibody Capture Enzyme-Linked Immunosorbent Assay (MAC-ELISA) test and molecular test like Nucleic Acid Amplification Test (NAAT) and polymerase chain reaction (PCR) like DENV-1-4 RT-PCR multiplex assay is done for detection and identification of particular serotype. However, all these facilities are not currently available in all clinical settings of Nepal. This is why detection of dengue cases takes time.
Health authorities of 20 countries have recommended Dengvaxia—the first vaccine against dengue—for patients of nine to 45 years. Preventive measures and supportive care are critical to management of dengue. It is necessary to maintain the patient’s body fluid volume in severe form of dengue. Avoiding mosquito bites and integrated mosquito management are equally crucial. Destroying the egg laying habitat (larval habitat) of mosquito by spraying larvicides have been quite effective in controlling mosquito. Use of neutral colored clothing, long sleeve if possible, proper screening of doors and windows, use of insect repellents during day time helps in avoiding mosquito bite that ultimately reduces the risk of having dengue infection. Additionally, insecticide-treated mosquito nets can prevent mosquito bites. Careful early clinical detection can significantly reduce dengue deaths. According to Epidemiology and Disease Control Division (EDCD), Kathmandu is at a high risk of dengue outbreak as it harbors a large number of dengue Aedes species mosquitoes. That’s why concerned stakeholders should immediately initiate the campaigns, with community participation, for sustained vector control of dengue virus. Government authorities should monitor the effectiveness of vector control interventions. Moreover, proper waste management and control of egg-laying habitats may reduce the egg-laying habitats of Aedes mosquitoes. Health notices, and warnings are also recommended to make public aware about dengue outbreaks.
Rayamajhee is a Research Faculty at Department of Infectious Diseases and Immunology of Kathmandu Research Institute for Biological Sciences. Bhandari is a Post Graduate Scholar at Department of Zoology, Amrit Science Campus
rayamajheebinod@gmail.com
alakabhandari2222@gmail.com
You May Like This

Agriculture Minister hospitalized after suffering from Dengue
KATHMANDU, Sept 5: Agriculture Minister Chakrapani Khanal has been admitted to Grande International Hospital in the capital after suffering from... Read More...

Private health centers charging exorbitant fee for dengue test
DHARAN, June 19: Private clinics and hospitals in Dharan are taking advantage of dengue outbreak by charging exorbitant fee for tests... Read More...

Dengue detected in teenage girl in Chitwan
CHITWAN, Aug 20: A teenage girl has tested positive for dengue in Chitwan district which has been battling with the... Read More...



Just In
- Nepal sets target of 120 runs for UAE in ACC Premier Cup
- Discussion on resolution proposed by CPN-UML and Maoist Center begins in Koshi Provincial Assembly
- RBB invites applications for CEO, applications to be submitted within 21 days
- Telephone service restored in Bhotkhola after a week
- Chemical fertilizers imported from China being transported to Kathmandu
- Man dies in motorcycle accident in Dhanusha
- Nepal face early setback as four wickets fall in powerplay against UAE
- Australian unemployment rate rises to 3.8 percent in March













Leave A Comment